England is beset by a post-pandemic surge in sexually transmitted infections (STIs), with experts suggesting the rise of dating apps, changing sexual appetites and older ‘silver swipers’ could be fuelling the rise.
Official data shows 401,800 cases were diagnosed — including in children as young as 13 — in England last year, up almost a third on 2020.
Spiking rates in young teenagers and pensioners have been partly blamed for driving the increase, which also saw gonorrhoea soar to the highest level ever recorded.
Some experts have pinned surging rates on a post-lockdown boom in people having condomless sex with new partners.
But others sexual health specialists today told MailOnline the reasons behind the alarming rise in STIs are ‘complex’.
Dr Emma Harding-Esch, an epidemiologist and STI expert at London School of Hygiene & Tropical Medicine said: ‘It’s important to note that the UK is not the only country seeing these trends — they are a global phenomenon.’
Here, MailOnline breaks down the potential causes behind each age category.
13-24 year olds
Official data shows the sharpest year-on-year STI rise was seen among kids aged just 13 to 14, with numbers up by almost a fifth (19.5 per cent) to 459 on the previous year.
But while rates among 15 to 19-year-olds and 20 to 24-year-olds remained high, 2023 saw them level off sitting below pre-pandemic levels.
Experts have suggested a digital dating revolution and sexting could be behind the overall high STI rates in younger people.
Dr Harding-Esch told MailOnline: ‘Dating apps have enabled people to find sexual partners locally more easily and quickly, meaning there is a much wider pool of potential sexual partners than for previous generations.
‘These apps, combined with international travel, further increase the geographical and numerical sexual network.
‘STIs do not respect country borders.’
Professor Daniel Richardson, an expert in sexual health and HIV medicine at Brighton University has also cautioned that sexual habits, and appetites, among young people was changing.
‘People are having more sex with drugs which lowers their inhibitions and they are more fluid about their behaviour in terms of having sex with either the opposite sex or the same sex,’ he told The Telegraph.
Last year UKHSA urged university students to wear condoms if having sex with someone new amid a sharp rise in gonorrhoea cases among under-24s.
Evidence has previously suggested use of condoms, which prevent 98 per cent of STI transmission when used effectively, is in decline.
In the US, annual surveys of risky behaviour among high school students show condom use has fallen significantly over the past 20 years.
Just 51.8 per cent of those surveyed in 2021 said they had used a condom last time they had sex, compared to 63 per cent in 2003.
Experts have also suggested schools’ fear of attracting controversy by teaching sex education may also be to blame for the sharp rise among children.
Dr Harding-Esch told MailOnline: ‘We need better sex education so people can have happy, healthy, sex.
‘As such, the proposed Government policy to increase the age at which sex education is taught, and to limit the content, is worrying.’
In November, the Children’s Commissioner for England, Dame Rachel de Souza also warned sex education teaching has become ‘weaker and weaker’.
She told The Times Health Commission: ‘We’re in the middle of this culture war about relationships and sex education but we’re not actually teaching our kids what they need to hear.’
Dame Rachel also warned young people were now ‘getting their sex education from TikTok‘ which was making them less safe.
25 to 34-year olds
Of all age groups STI cases have long been highest among 25 to 34-year-olds. But the reasons why may now be changing, experts say.
Latest UKHSA data shows 137,515 cases were logged among this age group in 2023, a rise of almost 10,000 on the previous year.
Some have blamed trendy fertility awareness apps for the spike, warning the contraceptive method fails to protect against STIs.
Official figures suggest thousands of British women are ditching hormone-based contraceptives like the Pill in favour of the tech.
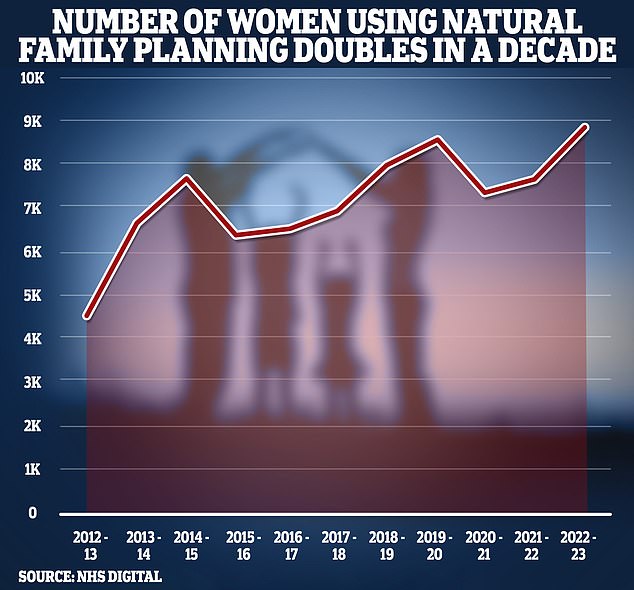
The numbers relying on natural ‘fertility awareness’, which involves tracking the menstrual cycle to find out when they are most likely to get pregnant, has doubled over the last decade.
But experts have warned many fertility apps are not supported by high-quality research and obviously don’t do anything to prevent STI transmission.
The NHS stresses that condoms are the only type of contraception that helps both prevent pregnancy and protect against STIs.


The number of women using natural family planning — monitoring cycle length, temperature and cervical mucus to predict when they are fertile — has doubled over the last decade, NHS figures show
Others also blamed rising infection rates among the young on a failure to notify and treat partners of people diagnosed with an STI who can continue to spread the infection.
Dr Harding-Esch told MailOnline: ‘There is little effectiveness in diagnosing and treating individuals with an STI if their partners are not also diagnosed and treated.
‘They will likely be re-infected and there will be continued onward transmission.’
STIs are an umbrella term for pathogens spread by sexual contact.
They include chlamydia, gonorrhoea and syphilis, are while often treatable can lead to serious health complications if left to develop.
These include pelvic inflammatory disease or chronic pain.
In extreme cases, chlamydia and gonorrhoea can even lead to infertility while syphilis can cause serious neurological and cardiovascular issues.
The NHS advises waiting 14 days after risky sexual contact before testing for chlamydia and gonorrhoea and four weeks for syphilis and HIV.
This is because it can take this long for levels of the pathogens to reach detectable levels in tests.
35 to 44 year-olds
Data suggest its not just the stereotypical younger Brits engaging in ‘increased risky sexual behaviour’ raising the risk of STIs.
UKHSA data show infection rates among 35 to 44-year-olds have exceeded the figures seen prior to Covid, with 59,017 recorded in 2023.
Dr Harding-Esch said: ‘There have been reports of an increase in the number and diversity of partners.
‘It’s therefore harder to target certain population groups with messaging and interventions.’
Brits have also seen a ‘broadening of sexual repertoires’ over the past 30 years, according to the British National Survey of Sexual Attitudes & Lifestyles.
The latest survey – which has collected data on the bedroom activities of the nation every 10 years since the late 1980s – shows the UK has become more accepting of non-monogamous relationships.
Involving 15,162 people aged 16-74 from across England, Wales and Scotland, it also suggested the number of partners people say they have had over their lifetime has increased.
In 1990-91, women aged 16-44 reported an average of 3.7 opposite sex partners, but this has risen to 7.7 two decades later.
Men, meanwhile, had an average of 8.6 opposite sex partners in 1990, then 12.6 in 2000 before dropping to 11.7 in the 2010s.
45 to 64-year-olds
Experts say the reasons behind a rise in STIs in the 45-to-64-year-olds are complicated.
UKHSA data shows cases rose by almost 5,000 in a year, hitting 34,535 in 2023. It marks a return to levels seen pre-pandemic.
Dr David Lee, an expert in ageing and disease on sexual health, from the University of Manchester told HuffPost it’s possible rising divorce rates mean a wave of over 50s are looking for new partners after long periods spent in committed relationships.
If women are post-menopausal, or men have undergone vasectomies, they sometimes dismiss the need to practice safe-sex, he added.
They may forget about STIs or naively dismiss them as something that only concerns young people — because this is what the messaging says.
Britain’s former chief medical officer Professor Dame Sally Davies also previously warned: ‘It is possible that women, particularly post-menopause, do not use condoms because they equate condom use with preventing pregnancy rather than prevention of STIs.’
So alarmed are health authorities by the trend that in 2019 one NHS trust in Derbyshire launched the ‘Jiggle Wiggle’ campaign.
This saw health staff handing out free contraceptives specifically to people in their 40s, 50s and 60s.
Condoms and other contraceptives were made available at food banks, GPs, pharmacies and other community venues across the county.
They also handed out at-home STI testing kits.


The proportion of women taking oral contraceptives has fallen by more than two-thirds, from 420,600 in 2012/13 to 126,400 in 2022/23, according to the NHS data. Around 555,400 women turned to the health service’s sexual and reproductive health services in 2022/23 — equivalent to four per cent of 13 to 54-year-olds. Of these, 8,800 confessed to using ‘natural family planning’ as their main method of contraception


Syphilis is sometimes called ‘the great pretender’ as symptoms are similar to other STIs. Here are five warning signs of the disease to look out for
65 years and older
Pensioners aged 65 and over, saw the second highest jump in STIs last year, with new cases soaring almost a fifth in a year to 2,885.
Figures show 558 cases of gonorrhoea were logged in this group in 2023 a 44 per cent rise on the 387 logged in 2019.
Chlamydia rates saw a similar rise more than a third (39 per cent) to 770 last year.
Experts have previously blamed the hike on so-called ‘silver swipers’, with dating apps like Tinder and Hinge enabling older people to meet new sexual partners more easily than in the past.
Sexual health awareness campaigns are often solely directed at young people, they have also warned.
This means many older daters simply don’t know they are at risk, especially if they only had a handful of partners when they were young.
And charities say the data may not even show the true extent of the issue.
Caroline Abrahams, director of the charity AGE UK told MailOnline many older people have never sought sexual health advice from their healthcare professional, either through embarrassment or not recognising the symptoms of STIs.
Instead, they ignore the problem and are not included in the data.
Ms Abraham added: ‘Sex continues to be a key part of life for many older people, and sadly the taboo around this topic means that older people with an active sex life are at greater risk of STIs than they need or ought to be.
‘Just like everyone else older people should be encouraged to practice safe sex particularly if they have multiple partners.
‘There are many stereotypes and myths about sex later in life and health professionals need to be open about discussing sexual health with older people and not jump to the conclusion that sex is irrelevant once you reach a certain age.’
She added: ‘Often public health messages surrounding safe sex are aimed at younger people, so they need to be clear that the risk doesn’t go away once you pass a certain birthday.
‘There is no age limit to having sex and that means there is no age limit to the risk of getting an STI.’
The rise has also meant NHS trusts have had to come up with innovative ways to tackle the problem.
In 2018, the Royal College of Nursing published a 44-page brochure – ‘Older People in Care Homes: Sex, Sexuality and Intimate Relationship’.
It said older people were still sexually expressing themselves, and nurses and care staff needed to acknowledge it within their care in a sensitive, legal and practical way.
Source: Mail Online